Patients require physical therapy for numerous reasons, including after an operation. Traditionally, post-op clients have been relegated to land-based rehab. The thought process governing this line of thinking was that aquatic therapy was not possible until their surgical sites had healed and any related conditions (e.g., incontinence, balance issues, mobility concerns) had been adequately eliminated.
Now, advanced and innovative hydrotherapy techniques and products have paved the way for extremely safe early intervention post-op. This not only produces faster patient healing, but lessens the problems associated with waiting to engage in physical therapy after a surgical procedure, such as:
- Patients become emotionally despondent and lose hope because they are unable to make progress. They enter into a cycle of fear avoidance, where they assume that when they finally do undergo physical therapy, they will feel pain. Early aquatic therapy may be one of the most reliable ways to help people avoid a downturn in their outlook after surgical procedures such as total knee replacement, back/spine surgery and hip replacement.
- Muscular atrophy takes place, which may make physical therapy more difficult or uncomfortable. When muscle groups are not used for a period of time, they begin to lose their ability to function. This is true not only for muscles affected directly by surgery, but also muscles that end up being unused after surgery. Thus, a shoulder surgery patient may see muscular atrophy in the arms and chest because of limited movements. Getting the patient into the water as soon as possible can significantly reduce this kind of negative conditioning. Additionally, increased range of motion (ROM) leads to improved post-op results and a quicker return to more normal activities of daily living.
- Erratic gait patterns and other problematic movements become the “norm” as patients try to make early strides without the guidance of a physical therapist. As individuals start to heal, they may “favor” one side of the body. This can cause abnormalities in the way they move. It can also lead to stress and strain. Water, a low weight-bearing environment, makes it easier for the patient to begin to move naturally and develop a normal, better-balanced gait.
Early aquatic therapy has been shown to remove many barriers to successful rehabilitation without compromising safety or progression when specific guidelines are followed. These guidelines fall under the categories of waterproofing, water chemistry and general best practices.
Reasons to Get an Early Start on Post-Op Hydrotherapy
The earlier your patients start hydrotherapy, the faster they will recover. Once the wound stops draining, patients should get in the water as soon as possible. Here are a few reasons not to delay aquatic therapy after surgery:
Encourages Safe Muscle Movements
Engaging in land-based exercises too soon after surgery could lead to further injuries. The buoyancy of water provides a safe environment for post-op patients to increase their mobility. Aquatic therapy improves muscle and joint functions without placing too much strain on wounded or injured areas.
Reduces Scarring
Hydrotherapy improves blood circulation, causing more blood to flow to the surgical site for faster healing and reduced scarring. The increased blood flow also prevents a buildup of surgical scar tissue under the skin.
Boosts Morale
When patients make progress early in their recovery period, it boosts their confidence and improves their mood, encouraging them to keep up with their aquatic exercises. These positive experiences are essential for athletes who may be out of action after surgery.
Maintains Fitness Level
In addition to encouraging athletes to continue their therapy, post-op hydrotherapy helps them maintain their fitness levels. Resuming physical activity soon after surgery results in smoother transitions as athletes get back into their regular training routine. In some cases, where patients are waiting long periods for surgery, patients may also benefit from aquatic therapy before surgery. Pre-op therapy can help reduce symptoms for patients with chronic pain.
Reduces Pain
Since water puts less weight on muscles and joints, patients experience less pain during and after their post-op aquatic therapy. Many patients notice immediate pain relief after engaging in hydrotherapy. Reassure your patients of this benefit to encourage them to start hydrotherapy soon after their surgical procedure.
Waterproofing Surgical Sites for Aquatic Therapy
The biggest physician concern is allowing patients who have recently had operations to get into water. The concern stems from the possibility of the wound becoming infected. However, proper wound waterproofing techniques enable physical therapy professionals to get their patients into the water faster without contaminating the wound.
After the wound is no longer draining, water therapy can begin. The first step to waterproofing is ensuring that the wound is completely covered in an occlusive waterproof dressing placed above a gauze pad. The gauze serves the purpose of providing physical proof that no water seeped into the dressing during the aquatic therapy session. By systematically focusing on completely sealing the wound area, physical therapists can ensure that their patients are water-ready.
“After five years of therapy we’ve found that we’ve had no infections to date that we can contribute to pool use. We monitor the wounds very closely, but the methods that we use to control the exposure of the wounds have been very effective in terms of preventing infection and keeping our wounds clean. In reviewing our numbers, we’ve had approximately 9,500 patient visits per year to the pool. We haven’t had any infections to this date.” – Dr. Robert P. Cusick of Kansas Joint & Spine Institute.
Support for safe waterproofing during early post-op aquatic therapy sessions comes from studies and documentation like “Early Aquatic Physical Therapy Improves Function and Does Not Increase Risk of Wound-Related Adverse Events for Adults After Orthopedic Surgery: A Systematic Review and Meta-Analysis” from the Archives of Physical Medicine and Rehabilitation. During this research involving 287 participants who engaged in aquatic therapy as early as one-week post-op, none of them experienced wound-related adverse effects that were any different from those expected with land-based therapy. Thus, the study concluded that aquatic therapy could be safely used during the early stages after orthopedic surgery.
How to Waterproof a Wound
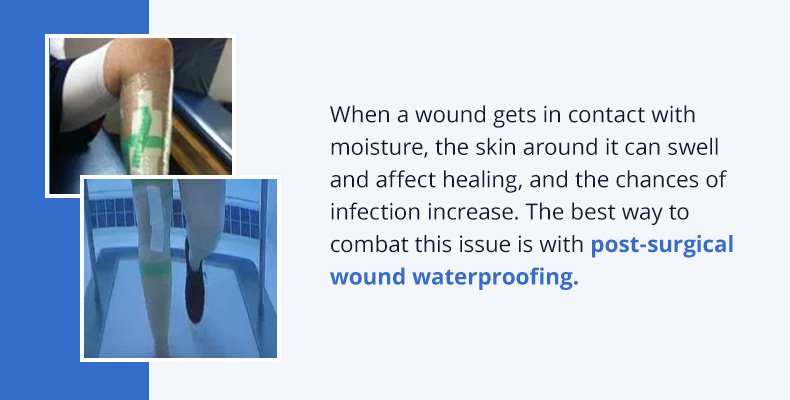
- Cut a piece of sterile gauze just larger than the size of the wound and lay it on the wound. This allows us to document that the wound stayed dry. The gauze goes on dry, stays dry, and is removed dry. This must be documented.
- Apply adhesive spray to the area that will receive the waterproof dressing.
- Apply the clear OpSite or Bioclusive dressing over the wound, being sure to anchor it well. Rub it down firmly and make sure it’s smooth. Seal the edges firmly. If this is done, when bending of the extremity occurs, there will not be breakage in the dressing.
- When the session is over, remove the dressing, touch the gauze to make sure it’s dry and document accordingly.
Regulating Water Chemistry Levels
It’s critical to maintain daily acceptable water chemistry levels of an aquatic therapy pool for the benefit of all patients, as well as physical therapists who join them in the water. Surgeons and physicians are more apt to recommend early aquatic therapy intervention when they know that a physical therapy clinic’s pool is being routinely checked and treated. Plus, post-op patients whose surgical sites have been sufficiently waterproofed will appreciate these measures.
Best Hydrotherapy Practices Related to Peripheral Patient Conditions
Some of the other questions about early post-op intervention in the water relate not to the pool itself, but to peripheral patient conditions. Notably, incontinence and limited mobility are often discussed.
Incontinence is a common occurrence among certain populations of post-op patients. In these cases, bowel and bladder issues have to be addressed before early rehabilitation – or any aquatic rehab – can take place. This can be done through pragmatic toileting practices, such as visits to the bathroom immediately before and after each aquatic therapy session. It may also be practical to talk about medications and other medical interventions that can reduce incontinence events.
Another best practice consideration involves patients who are wheelchair-bound or bed-bound after surgery. Getting these individuals into an aquatic therapy pool safely requires special training and measures. Many HydroWorx pools and stand-alone units offer unique ways of getting patients into the water straight from a wheelchair or a special chair lift.
Research Shows Earlier Intervention Helps Patient Progressions Post-op
Researchers from Australia’s Allied Health Clinical Research Office, Eastern Health and School of Physiotherapy and La Trobe University studied the results of 287 adult patients (weighted mean age of 65) who were placed into aquatic environments for therapeutic and rehabilitative regimens within 4-14 days post-surgery. Their thorough analysis found that early aquatic interventions did not increase the risk of wound-related adverse effects. In fact, there was a noted increase in pain reduction, decrease in edema, increase of strength and improvement of range of motion in the earlier postoperative stages when patients were given the opportunity to rehab in a warm water therapy pool. This enabled them to start to recover faster and move to land-based physical and occupational therapies.
The faster hydrotherapy can be initiated, the better the patient outcome. By taking sensible, proven steps ahead of time, a physical therapy professional can reliably work with post-op patients in aquatic atmospheres for excellent results. When a positive, safe foundation is laid, amazing achievements are possible. It all begins with the right mix of aquatic tools necessary to promote healing.
Here at HydroWorx, we provide quality aquatic wellness pools ideally suited for post-op hydrotherapy. Our pools come with underwater treadmills and moveable floors to help patients ease into their aquatics program. Contact us for more information on our pools and how they can assist your post-op patients.

