Parkinson’s Disease Aquatic Therapy Helps Patients
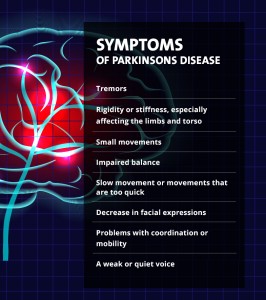
Parkinson’s disease is a chronic and progressive disorder that impacts movement and coordination. Symptoms happen because of the loss of neurons and decrease in dopamine production in the brain. Patients with Parkinson’s can have many different symptoms, including:
- Tremors
- Rigidity or stiffness, especially affecting the limbs and torso
- Small movements
- Impaired balance
- Slow movement or movements that are too quick
- Decrease in facial expressions
- Problems with coordination or mobility
- A weak or quiet voice
The brain has important brain cells called neurons, which are responsible for sending information to gland cells, nerve cells and muscle cells. Parkinson’s causes some neurons to function incorrectly and die.
The condition especially affects the neurons in the substantia nigra, an important part of the brain. The neurons affected by Parkinson’s produce dopamine. This chemical sends information related to coordination and movement, which is one reason why patients with this condition have trouble controlling the movement of their bodies.
Helping People With Parkinson’s Disease
According to the Parkinson’s Disease Foundation, nearly one million Americans live with the condition. Worldwide, 7-10 million people are affected and about 60,000 new cases are diagnosed in the United States each year. In addition to diagnosed cases, thousands of Americans live with Parkinson’s without knowing it.
According to the foundation, aging is an important risk factor for Parkinson’s disease. There is a two to four percent risk for Parkinson’s among people over age 60, compared with one to two percent in the general population. The average age at which the condition is diagnosed is 62, and as the baby boomer generation ages it is expected that diagnoses of Parkinson’s may double.
Scientists do not know exactly what causes the condition, and there is no known cure. In many cases, people who are diagnosed with the condition are given medication or are treated with surgery. While these options do not treat the condition, they can improve quality of life and can help manage symptoms.
Some patients are choosing to improve the quality of their life and their overall health to manage symptoms. To do this, patients are turning to:
- Natural supplements such as:
- Vitamin E
- Creatine
- Vitamin C
- Therapies such as:
- yoga
- meditation
- aquatic therapy
In many cases, these types of Parkinson’s disease therapy solution can be combined with medication and surgery or can be used alone to help manage symptoms.
What is Water Therapy?
Aquatic therapy refers to any exercise or therapy that is conducted in a controlled and monitored water environment — usually a pool. For example, aquatic exercise inside a pool, usually a heated pool, can involve exercise to improve fitness levels or overall conditions. Aquatic physical therapy involves physical therapists using physical therapy protocols in a pool or water setting.
Aquatic therapy can be used to help patients with cardiovascular conditions, minor injuries and serious illnesses such as Parkinson’s. Even generally healthy patients and high-endurance athletes turn to this form of therapy to improve endurance and to rehabilitate various injuries.
History of Water Therapy
Water therapy has been used since ancient times, dating back to 400 BC and potentially earlier. By the 17th and 18th centuries, scientists were considering the chemical components that could make this type of therapy more effective, and by the 19th century there was interest in varying the temperature of the water to improve efficiency. For centuries, natural heated springs and spas were a solution for those suffering a variety of ailments, and doctors prescribed “taking the waters” to deal with pain and discomfort.
Today, water therapy continues to be a widely recognized form of therapy for many conditions, including Parkinson’s disease. In 2005, $46 million was spent on aquatic therapy in the United States and accounted for about 3% of the codes billed to Medicare.
Parkinson’s Disease Aquatic Exercise: What You Need to Know
People with Parkinson’s disease who exercise regularly move and maintain balance better than those who do not. Water boasts unique properties that enable it to be used for both therapy and fitness, especially for persons who cannot comfortably move on land, as is often the case for people with Parkinson’s.
Reducing a Fear of Falling
In water, the fear of falling evaporates. The biggest danger to people with gait and balance issues, gravity, is simply not an issue in the pool. The buoyance of the water can make fear of falling much less. Even if a patient does stumble, the risk of injury is minimal.
Aquatic therapy equipment, such as HydroWorx therapy pools, comes with support bars and other tools to offer added assistance for those who require it. The pool becomes a safe and supportive place for therapy and exercise. Patients can work with physical therapists with the added confidence of knowing falling is less likely and there are bars and other safety protocols in place to help them even if they do lose balance temporarily.
Water’s buoyancy immediately renders anyone submerged to feel lighter than he or she would on land. Depending upon the level of submersion, up to 80-90 percent of a client’s body weight could be counteracted. Thus, a 200-pound man would move as if he only weighed 20-40 pounds. As a result, his movements would take less effort than if he were doing the same movements in a land-based environment.
Easier Movements
The assistance of buoyancy allows for bigger movements. Clients can practice walking with a more normal or exaggerated gait and carry out progressively larger ranges of motion. At the same time, forces of resistance and turbulence challenge balance and coordination. In addition, the soothing, warm temperature relaxes muscles and helps lessen rigidity and pain. When someone with Parkinson’s is able to float and move in a pool, they feel so much freer than on land. Participants can stand up tall, with increased truck extension and move more freely.
Parkinson’s patients most notably suffer from tremors, and water can assist with this as well. A warmer pool can soothe muscles while the natural resistance of the water relaxes movements. Tremors are lessened and patients have more time to respond and focus on movement.
Since the water is often kept warmer in these sessions, it is important to keep the air warmer as well for comfort and to prevent shivering. Offering clothing or a covering when patients get in and out of the pool can also help keep patients comfortable.
Aquatic therapy offers the added benefit of hydrostatic pressure, or the force exerted by the water on the body. Even patients who have more advanced Parkinson’s can enjoy some of the benefits of being submerged in an aquatic therapy pool. Hydrostatic pressure can:
- Reduce swelling
- Reduce pain
- Help the heart and boost circulation
- Reduce sensory input to the brain
- Reduce the pooling of blood in the extremities
For all these reasons, even someone who is new to aquatic therapy and exercise may find some benefit and relief simply by getting into the pool. Physical therapists can use this initial improvement to motivate a patient to try exercises and movements the patient thought were not possible for them.
In the water, low-impact exercise is possible and is easier to achieve. On land, each step may cause stress on joints, muscles, and tissues, but in the water the buoyancy naturally creates less stress on the muscles and the body. Patients who cannot easily move on land sometimes find their mobility much easier in the water. At the same time, the water provides some resistance to improve the effectiveness of exercises.
Since Parkinson’s patients may worry about falling and about movement, this can prevent them from exercising. The reluctance can mean muscles weaken further without exercise, leading to even smaller ranges of movement.
Patients who don’t bear weight and attempt to exercise may find themselves moving less, eventually losing confidence and independence. With Parkinson’s disease exercise programs in an aquatic therapy setting, patients feel more comfortable, which can encourage them to exercise so they can gradually build up strength.
A Range of Exercises
A range of Parkinson’s disease therapy exercises are possible with aquatic therapy. Let’s run through the most important ones.
Standing Exercises
Patients can try standing and stretching in place or marching to improve core strength. Focus on posture can also help build strength and postural stability, which can be an issue for those living with Parkinson’s disease.
Strengthening Exercises
Leg lifts are made easier with the buoyancy of the water and can help strengthen muscles to improve walking and mobility. Hip extension exercises and walking on the treadmill can improve posture and mobility. Physical therapists can lower or raise the water levels in therapy pools so that patients who are working on postural and leg exercises in the water can be half-submerged.
Walking Exercises
To help with walking, patients can be submerged further. At first, patients may want to hold onto the support bars for balance, but with time patients find they may be able to walk without the assistance of the bars, especially when submerged up to the neck. As patients work on simple movements and walking, they can slowly regain agility, balance and coordination. Patients can walk:
- Backward
- Forward
- With side steps
These exercises encourage a range of movements to improve posture and flexibility. With each repetition, endurance and strength improve.
As patients improve their walking and movement, they can enjoy the benefits of a low-impact aerobic exercise in the pool. This is especially important for Parkinson’s patients, who may get less aerobic exercise if they worry about falling or experience mobility problems.
Without aerobic exercise, patients may find they experience overall weakness or loss of conditioning. Lack of aerobic exercise can also lead to higher blood pressure or heart health issues over time. Aquatic therapy puts aerobic exercise within reach for many Parkinson’s patients, allowing them to reap the reward of this type of exercise.
Stretching Exercises
Yoga, Pilates and other exercise modalities are also very possible in an aquatic therapy setting and potentially offer plenty of benefit to Parkinson’s patients. Both yoga and Pilates encourage a range of movements and deep breathing exercises that can build confidence, flexibility and strength.
On land, these exercises can be very intimidating for Parkinson’s patients but they become more possible when adapted for therapy pools because the buoyancy of the water supports patients as they try new movements. Pilates, yoga and other exercises can also be very effective in the water because the water offers natural resistance, making the muscles and the heart work harder to get through the resistance.
Request a Free Info Kit View Our Products Find a Pool Near You
Whole-Body Healing
Since movement in the water is easier than it is on land, patients immediately get a confidence boost once they see movement is easier than they expected. Confidence in the pool can lead patients to try more exercises and movements.
One of the big challenges with patients who have Parkinson’s and other chronic conditions is patients may suffer a range of disappointments. Patients may have tried exercises or movements and not been successful, making them reluctant to try again because they believe they “can’t” do a specific move. Water therapy and exercise can show patients they can, which can make them more cooperative to try different Parkinson’s disease exercise protocols.
Aquatic environments are also a great place to move facial muscles, practice breath control and vocal volume. Often, clients enjoy creating an echo, blowing bubbles or ping pong balls across the pool. Counting repetitions forward or backward by twos and threes, quickly changing directions on command, and discussing historical or current events specifically stimulate the brain while exercising.
The combination of social, mental and physical activity in aquatic therapy can help Parkinson’s patients. Patients who try this type of therapy report:
- A wider range of movement
- Better stability
- Greater independence
- Increased confidence
- Better quality of life
One of the things that can be frustrating about a Parkinson’s diagnosis is patients are told the condition is chronic and progressive. Patients worry there is no cure and they will slowly lose independence. With aquatic therapy and exercise, patients can see they are managing symptoms and in some cases improving mobility and function, improving their outlook as they improve their physical condition.
Water-based therapy can also encourage patients to keep moving. According to neurologist Dr. Lynn Struck of Iowa Parkinson Disease Information and Referral Center, among patients who exercise and stay fit early on, motor skills and mobility can be preserved for longer and at a higher level. In addition to intangible benefits, Parkinson’s disease exercise therapy and aquatic therapy offer real, tangible benefits.
There may be other, less tangible benefits for patients who try aquatic therapy:
- Group classes can encourage socializing, which can reduce the risk of anxiety, depression and isolation that chronic disease can sometimes cause.
- Exercise has been shown to reduce stress and to improve confidence, which is also useful for patients suffering from a serious disease such as Parkinson’s Disease.
- Aquatic therapy can be relaxing and soothing, which is important in reducing the stress and possible emotional upset of living with a serious condition.
Just as healthy patients will feel soothed by climbing into a warm bath and anyone can feel more relaxed by floating in a pool on a warm day, patients with Parkinson’s can experience the tranquility that comes with being safely submerged in warm water.
For physical therapists, aquatic therapy pools offer a range of tools that can help them assist patients. HydroWorx pools, for example, offer:
- Underwater video monitoring
- Adjustable depth
- Moveable floors that double as an underwater treadmill
- Therapy and resistance jets
- Hydromassage
Many physical therapists and doctors recommend a water-based Parkinson’s disease exercise program for patients. In fact, the American Parkinson Disease Association has recommended aquatic therapy as a good option for Parkinson’s patients.
Things to Consider With Parkinson’s Disease Aquatic Exercise
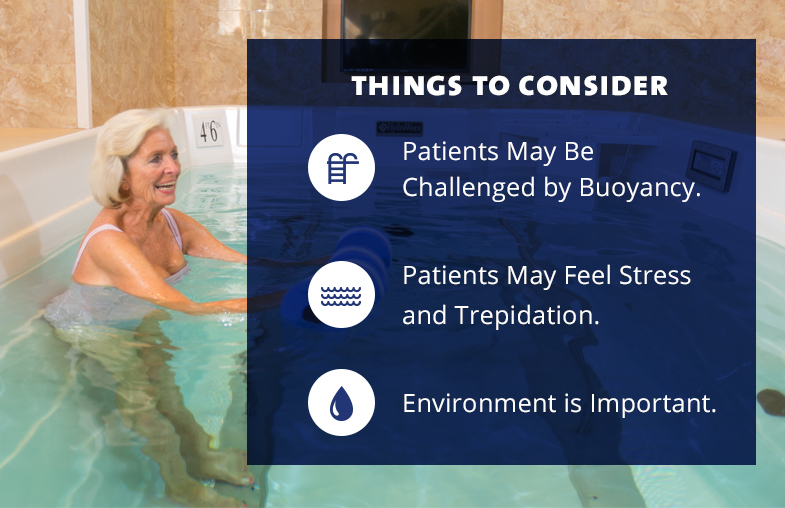
Although aquatic therapy offers a range of benefits for Parkinson’s patients, there are a few things physical therapists, athletic trainers and group fitness instructors will want to consider when leasing or buying Parkinson’s disease exercise equipment and offering aquatic therapy.
1) Patients May Be Challenged by Buoyancy
While buoyancy in the pool can make movement easier and can strengthen the core, it can also offer a challenge for patients just starting out and patients who have weakened or spastic muscles and extremities. This can cause balance problems in the pool. Using grab supports or float supports can help, especially as patients slowly gain strength and confidence.
2) Patients May Feel Stress and Trepidation at First
Patients who have already tried a number of therapies without success may not have high expectations. Some may worry whether they can stay safe in the pool with a limited range of movement. For many people with physical challenges caused by Parkinson’s and other conditions, simply being seen in a bathing suit by others can be stressful.
There are many things that can help patients with these concerns. Testimonials from other patients and more information about aquatic therapy can help. Explaining the therapy pool, Parkinson’s disease therapy protocol, and exactly what will happen in and out of the pool can also be useful. Open communication, sensitivity and humor can help patients overcome trepidation, shyness and worry in many cases.
3) Environment is Important
In addition to developing a Parkinson’s disease physical therapy protocol and leasing or buying the needed equipment, creating the right environment is important. Creating a pleasant therapy area and offering plenty of time for questions and treatment can be helpful. Colors and music can create a pleasant and relaxing environment. A good balance of privacy and support can also help patients feel more comfortable.
How Effective is Parkinson’s Disease Aquatic Therapy?
A number of exercise research studies have shown Parkinson’s disease aquatic therapy can be very effective, even when compared with other types of Parkinson’s disease exercises and therapies.
For example, a 2011 research study published in the Archives of Physical Medicine and Rehabilitation compared Parkinson’s disease aquatic therapy and land-based Parkinson’s disease therapy. The study’s authors concluded postural stability improved “significantly” more for patients using aquatic therapy.
In 2013, Brazilian researchers published a study in the journal Advances in Parkinson’s Disease. The researchers examined Parkinson’s patients before and after aquatic therapy and concluded that motor skills of the patients improved after Parkinson’s disease aquatic exercises in a heated pool.
A 2012 study published in Gait & Posture found patients who worked with aquatic exercise programs showed better hip angle, gait, speed and stride length. Many other studies have supported these findings, concluding aquatic therapy and exercise are an effective way to assist Parkinson’s patients. Some studies have also concluded aquatic therapy is effective for Alzheimer’s and other serious conditions as well.
Watch and learn how aquatic therapy has helped this Parkinson’s patient:
Finding Out More About Parkinson’s Disease Exercise Recommendations
If you’d like to see the power of Parkinson’s disease physical therapy and aquatic therapy for yourself, request a free informational kit from HydroWorx to learn more about owning or leasing a therapy pool. You can also browse the HydroWorx website to find out more about aquatic therapy research and find other resources that can help clinicians maximize the properties of water and creatively challenge clients with Parkinson’s disease.
Bigger is Better: Aquatic Exercise Benefits People with Parkinson’s Disease, a free webinar, presented by Cathy Maloney Hills and Christine Shidla on March 21, 2013 from 2 to 3pm EST.
This webinar will provide tools for therapists, personal trainers and group fitness instructors to maximize the properties of water and creatively challenge clients with Parkinson’s disease. ICAA Members can watch the webinar on demand here>>
SPEAKER BIOS:
Cathy Maloney-Hills, RPT, is an aquatic physical therapist working for Courage Center at Summit Place Senior Campus, Eden Prairie, MN and Heritage Park Senior Services Center in Minneapolis, MN. She is co-investigator/author for the study and program: Golden Waves® Functional Water Program for Older Adults, University of Nevada, Reno and a co-author of the YMCA Water Fitness for Health.
Christine Shidla is the Director of Wellness at Summit Place Senior Campus, Eden Prairie, MN. She is also a trainer and speaker for exercise for the Arthritis Foundation. Christine received her Bachelor of Science Degree in Kinesiology, with emphasis in Sports Medicine, from the University of Minnesota.
Page updated on: July 7th, 2020





Aquatic therapy sounds interesting. I wish I could send my mother to aquatic therapy classes somewhere near in the Kansas city. For treating her Parkinson’s, she is going to Rock Steady Boxing Classes regularly but I want her to do more for her Parkinson’s disease so that she could live longer and healthy with Parkinson’s disease.
Please check out our new locator to see if there are any facilities nearby for your mother: https://www.hydroworx.com/contact/locations/
I wish that I could go for the aquatic therapy in Sydney. I want to be a healthy and strong person for my family. The Parkinson disease is making me weaker day by day.
My friend finds the public pools in Canada too cool which starts the tremmers. Are there any swim suits or products that will help keep her warmer.
A warm water pool is ideal. I am not sure of any specific products that could be used to help with the water temperature.
I don’t think it’s enough that my father’s doctor has recommended medication and surgery to help manage symptoms as you pointed out of my father’s Parkinson’s disease so I might ask him to go to therapy as well. Since you said that aquatic therapy is exercise, I think he will benefit from it since he needs to move his body more. If he will be able to maintain his balance better than those who do not as you said, I’ll consider asking if anyone is offering this type of therapy in their clinics or if there are any other suitable alternatives as well.
In North Vancouver Canada there is a fantastic Parkinsons programming Lynn Valley at The Molly Nye House. It is called PWR4life with Surefeet and it is on Monday and Wednesday at 4-5. In West Vancouver at the WV Aquatic Center on Tuesday and Thursday 1:30-2:30 there is a Parkinsons Aquatic class in warm water taught by 2 rehabilitation specialists .
Do you have a printable list of aquatic exercises for a newly diagnosed Parkinson patient? I am his caregiver and am familiar with the balance excercises, walking, one foot on the ground etc but would love some guidance.
Unfortunately, we do not have a printed list available right now, but we will see if there is something we can share via email!